Understanding Cerebral Amyloid Angiopathy (CAA)
Cerebral Amyloid Angiopathy (CAA) is a significant neurological condition characterized by the deposition of amyloid proteins in the walls of cerebral blood vessels. This condition is prevalent in the elderly and is a major cause of lobar hemorrhages and cognitive decline. The research article titled Updated Outlook of Cerebral Amyloid Angiopathy and Inflammatory Subtypes: Pathophysiology, Clinical Manifestations, Diagnosis and Management provides a comprehensive review of CAA, offering valuable insights for practitioners.
Key Findings and Implications for Practitioners
The research highlights several critical aspects of CAA, including its pathophysiology, clinical manifestations, and management strategies. Understanding these elements is crucial for practitioners aiming to improve their diagnostic and therapeutic approaches.
Pathophysiology and Clinical Manifestations
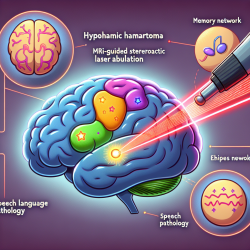
CAA is primarily caused by the deposition of insoluble amyloid proteins in cerebral blood vessels, leading to vessel fragility and potential hemorrhages. The condition can present with a range of symptoms, including transient focal neurological deficits, commonly referred to as "amyloid spells," which can be misdiagnosed as seizures or transient ischemic attacks.
Diagnostic Criteria
The diagnosis of CAA relies on imaging techniques such as CT and MRI, with the Edinburgh and Boston Criteria providing frameworks for diagnosis. These criteria emphasize the importance of identifying specific radiological signs that correlate with CAA.
Management Strategies
Effective management of CAA involves addressing the underlying amyloid deposition and mitigating risk factors such as hypertension. The research underscores the importance of controlling blood pressure to reduce the risk of hemorrhage. Additionally, the role of immunosuppressive therapy in managing inflammatory subtypes of CAA is explored, highlighting the need for personalized treatment plans.
Encouraging Further Research
While the research provides a robust foundation for understanding CAA, it also identifies areas where further investigation is needed. Practitioners are encouraged to engage in ongoing research to explore new diagnostic tools and therapeutic interventions. This continuous learning process is essential for improving patient outcomes and advancing the field of neurology.
Conclusion
For practitioners in the field of speech-language pathology and neurology, the insights from this research are invaluable. By integrating these findings into clinical practice, practitioners can enhance their diagnostic accuracy and develop more effective management strategies for patients with CAA. To delve deeper into the research, please refer to the original article linked above.