The complex nature of schizophrenia often presents challenges for practitioners aiming to provide effective treatment. A recent study titled A cross-sectional study of current and lifetime sexual hallucinations and delusions in Lebanese patients with schizophrenia: frequency, characterization, and association with childhood traumatic experiences and disease severity offers valuable insights into this intricate disorder. By understanding the prevalence and associations of sexual hallucinations and delusions in schizophrenia patients, practitioners can enhance their skills and improve patient outcomes.
Understanding the Study
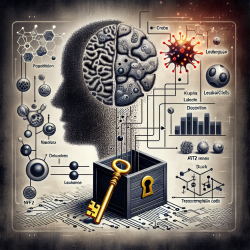
The research conducted in Lebanon involved structured interviews with 167 chronic schizophrenia patients. The study aimed to identify the frequency of sexual hallucinations and delusions and their associations with childhood trauma, illness severity, and substance use disorders. Notably, 36.5% of participants reported current episodes of sexual delusions or hallucinations, while 50.3% had experienced them at some point in their lives.
Key Findings
- Prevalence: Sexual psychotic symptoms were prevalent among the participants, indicating a significant area of concern for practitioners.
- Childhood Trauma: There was a strong association between childhood emotional and sexual abuse and the occurrence of sexual hallucinations and delusions.
- Substance Use: Alcohol consumption was linked to an increased likelihood of experiencing these symptoms.
- Disease Severity: More severe schizophrenia symptoms were correlated with higher chances of experiencing sexual psychotic symptoms.
- Education Level: Patients with higher education levels were less likely to experience these symptoms, suggesting that education may play a protective role.
Implications for Practitioners
The findings underscore the importance of screening for childhood trauma and substance use disorders in schizophrenia patients. Practitioners should consider incorporating trauma-informed care approaches to address these underlying issues. Additionally, interventions aimed at reducing alcohol consumption could potentially mitigate the risk of psychotic symptoms.
Cognitive-behavioral therapies that focus on addressing dysfunctional cognitive schemas related to sexual hallucinations and delusions may also be beneficial. By understanding the cultural context of these symptoms, practitioners can tailor their approaches to better meet the needs of diverse patient populations.
The Path Forward
This research highlights the need for further studies to explore the biopsychosocial mechanisms underlying these associations. Practitioners are encouraged to engage in ongoing education and research to stay informed about emerging insights into schizophrenia treatment.