Introduction
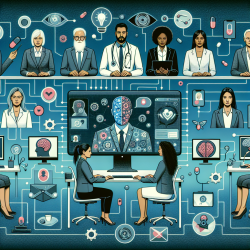
The integration of precision medicine into clinical practice has revolutionized the treatment of brain tumors, offering new avenues for personalized patient care. A recent research article, "Clinical and research applications of a brain tumor tissue bank in the age of precision medicine," highlights the importance of organized tissue banking in advancing our understanding of central nervous system (CNS) tumors. This blog aims to guide practitioners in improving their skills by implementing the outcomes of this research or encouraging further exploration.
The Role of Tissue Banks in Precision Medicine
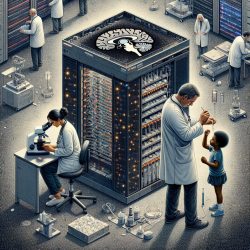
Tissue banks serve as a cornerstone for precision medicine by systematically collecting and storing brain tumor specimens. These repositories provide invaluable resources for molecular and genetic analyses, which are crucial for developing targeted therapies. The Hermelin Brain Tumor Center at Henry Ford Health System exemplifies the successful integration of a multidisciplinary team in managing a comprehensive tumor bank.
Key Takeaways for Practitioners
- Multidisciplinary Collaboration: Successful tissue banking requires collaboration among neuro-oncologists, surgeons, pathologists, and data scientists. Practitioners should foster a team-based approach to ensure seamless integration of clinical and research efforts.
- Standardized Protocols: Implementing standard operating procedures for specimen collection and handling is crucial for maintaining tissue quality. Practitioners should advocate for regular training and adherence to these protocols to ensure consistency.
- Data Integration: Linking clinical data with molecular findings enhances the potential for discovering predictive biomarkers. Practitioners should utilize bioinformatics tools to analyze and integrate data from tissue banks, facilitating informed clinical decisions.
Encouraging Further Research
While the current research provides a robust framework for tissue banking, there are opportunities for further exploration. Practitioners are encouraged to engage in studies that focus on:
- Longitudinal Data Collection: Expanding tissue banks to include longitudinal samples can provide insights into tumor evolution and treatment response over time.
- Patient-Derived Models: Developing patient-derived xenografts and cell models can enhance the understanding of tumor heterogeneity and aid in preclinical studies.
- Digital Phenotyping: Incorporating patient-reported outcomes and data from wearable devices can offer additional dimensions to precision medicine research.
Conclusion
By embracing the principles of precision medicine and leveraging the resources of brain tumor tissue banks, practitioners can significantly improve patient outcomes. The integration of multidisciplinary collaboration, standardized protocols, and data-driven decisions will pave the way for advancements in neuro-oncology.
To read the original research paper, please follow this link: Clinical and research applications of a brain tumor tissue bank in the age of precision medicine.