Introduction to Simulation in Integrated Care
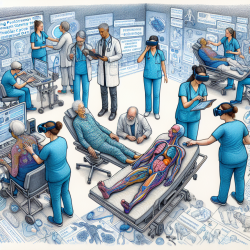
In the realm of healthcare education, the integration of simulation-based learning has emerged as a pivotal tool in enhancing the understanding of complex care systems. The research article titled "Using Simulation to Explore Medical Students’ Understanding of Integrated Care within Geriatrics" provides valuable insights into how simulation can transform medical education, particularly in the context of integrated care (IC) for geriatric patients.
Understanding the GPS-Care Experience
The "Getting to Know Patients’ System of Care" (GPS-Care) is a simulation program designed to immerse medical students in the intricacies of integrated care. Through role-playing as elderly patients or caregivers, students navigate a series of simulated healthcare appointments. This experiential learning approach allows students to grapple with the complexities of managing co-occurring physical and mental health conditions, thereby deepening their understanding of IC.
Key Outcomes and Themes
The research identified several key themes that emerged from the GPS-Care experience:
- Complex Care Experiences: Students reflected on the challenges of managing multiple health conditions simultaneously and the importance of addressing both physical and mental health needs.
- System of Care Reflection: Participants gained a greater appreciation for interdisciplinary teams and the need for effective communication and coordination among healthcare professionals.
- Understanding Integrated Care: The simulation highlighted the importance of navigating healthcare systems and the role of productive struggle in enhancing comprehension of IC concepts.
- Aspiration to Improve Care: Students expressed a desire to implement their learnings in future practice, focusing on holistic care and better integration of services.
Implications for Practitioners
For practitioners, the findings of this study underscore the value of incorporating simulation-based learning into professional development. By engaging in simulations like GPS-Care, practitioners can enhance their skills in managing complex patient needs, improve interdisciplinary collaboration, and foster a deeper understanding of integrated care models.
Encouraging Further Research
The transformative impact of the GPS-Care simulation suggests that further research into simulation-based learning could yield additional insights into effective educational strategies. Practitioners are encouraged to explore similar simulation programs and consider integrating them into their training curricula to enhance the quality of care provided to geriatric patients.
Conclusion
The integration of simulation in medical education offers a powerful mechanism for improving understanding and implementation of integrated care. By fostering productive struggle and reflective learning, simulations like GPS-Care can significantly enhance practitioners' ability to navigate complex healthcare systems and deliver holistic patient care.
To read the original research paper, please follow this link: Using simulation to explore medical students’ understanding of integrated care within geriatrics.