Introduction
The biopsychosocial model (BPSM), introduced by George Engel in 1977, has become a significant framework in medical research and practice. However, its application has been subject to criticism for lacking scientific content, leading to what some scholars describe as "wayward discourse." This blog will explore how practitioners can enhance their skills by critically examining the BPSM and its implications for practice, particularly in the context of speech-language pathology and child outcomes.
The Biopsychosocial Model: An Overview
The BPSM proposes that health and disease are products of interactions among biological, psychological, and social factors. While it has been praised for broadening the scope of medical inquiry beyond the biomedical model, critics argue that it lacks the scientific rigor needed to provide explanatory power. This has led to its misuse in medical discourse, where it is sometimes treated as a scientific model with explanatory capabilities it does not possess.
Wayward Discourse: A Cautionary Tale
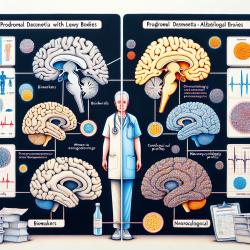
One of the key criticisms of the BPSM is its role in fostering "wayward discourse," where researchers make claims about diseases based on specious arguments. These arguments often rest on question-begging, appeals to authority, and conceptual errors. For example, some researchers have used the BPSM to assert that certain conditions, like temporomandibular disorder (TMD) and irritable bowel syndrome (IBS), are diseases with specific etiologies, despite lacking compelling scientific evidence.
Implications for Practitioners
For practitioners, especially those working with children, it is crucial to approach the BPSM with a critical eye. Here are some strategies to enhance practice:
- Understand the Limitations: Recognize that the BPSM is a conceptual framework, not a scientific model. It should not be used to define diseases or establish causality.
- Focus on Evidence-Based Practice: Prioritize interventions and assessments that are supported by robust empirical evidence. Use the BPSM to guide holistic understanding but not as a sole basis for clinical decisions.
- Encourage Interdisciplinary Collaboration: The BPSM highlights the importance of considering multiple factors in health outcomes. Collaborate with professionals from various disciplines to address the complex needs of children.
- Promote Conceptual Rigor: Be vigilant about the language and concepts used in practice. Avoid using the BPSM to make unfounded claims about disease etiology or treatment efficacy.
Conclusion
While the BPSM offers valuable insights into the multifaceted nature of health and disease, practitioners must be cautious of its limitations. By maintaining conceptual rigor and focusing on evidence-based practice, we can better serve the needs of children and contribute to more effective and scientifically sound medical discourse.
To read the original research paper, please follow this link: The biopsychosocial model: Its use and abuse.