Introduction
Obsessive-Compulsive Disorder (OCD) is a significant mental health challenge that affects millions globally. Cognitive-behavioral therapy (CBT) has been recognized as a first-line treatment for OCD due to its efficacy in symptom reduction and long-term benefits. However, access to CBT remains a substantial barrier, with only a small fraction of patients receiving this evidence-based treatment. A recent study by O'Neill and Feusner (2015) sheds light on innovative approaches to overcome these barriers, particularly through the use of neuroimaging to predict long-term outcomes.
Understanding the Barriers
The study highlights several barriers to accessing CBT for OCD, including:
- Stigma and Awareness: Many patients are unaware of CBT or are hesitant due to the stigma surrounding OCD.
- Shortage of Trained Therapists: There is a lack of therapists trained in CBT, leading to long wait times.
- Cost and Insurance Issues: The high cost of CBT and complexities in insurance coverage further limit access.
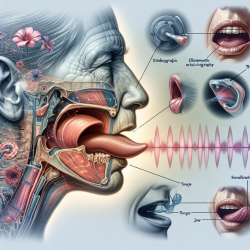
The Role of Neuroimaging
Neuroimaging, particularly resting-state functional MRI (rsfMRI) and magnetic resonance spectroscopy (MRS), offers promising avenues to predict the long-term success of CBT in treating OCD. The study suggests that these imaging techniques can identify biomarkers that correlate with treatment outcomes, potentially guiding personalized therapy plans.
Implications for Practitioners
For practitioners, integrating neuroimaging into the treatment planning process could enhance the precision of therapy delivery. By identifying patients who are more likely to benefit from CBT, therapists can optimize their resources and improve patient outcomes. This approach also holds promise for advocating insurance coverage by demonstrating the likelihood of successful treatment outcomes.
Encouraging Further Research
While the study presents compelling data, it is crucial for practitioners and researchers to continue exploring these findings. Further research could focus on refining neuroimaging techniques, expanding sample sizes, and validating results across diverse populations. By doing so, the field can move closer to a future where CBT is more accessible and tailored to individual needs.
Conclusion
Enhancing access to CBT for OCD through innovative approaches like neuroimaging not only promises better patient outcomes but also represents a step forward in mental health treatment. Practitioners are encouraged to stay informed about these advancements and consider their potential applications in clinical settings.
To read the original research paper, please follow this link: Cognitive-behavioral therapy for obsessive–compulsive disorder: access to treatment, prediction of long-term outcome with neuroimaging.