The human brain is a remarkable organ, capable of adapting and reorganizing itself in response to various stimuli and injuries—a phenomenon known as neuroplasticity. Recent research has provided new insights into this dynamic process, particularly through studies involving patients with gliomas. These insights offer valuable opportunities for practitioners to enhance their therapeutic approaches and improve patient outcomes.
The Power of Neuroplasticity
Neuroplasticity refers to the brain's ability to reorganize itself by forming new neural connections. This capability is crucial not only during normal development but also in response to injury or illness. For practitioners, understanding the mechanisms of neuroplasticity can lead to more effective therapeutic interventions.
A study titled Neuroplasticity: Insights from Patients Harboring Gliomas, highlights how glioma patients—often considered a less-studied group—can provide significant insights into brain reorganization mechanisms. Despite lesions in critical areas such as Broca's or Wernicke's area, many glioma patients do not exhibit detectable language deficits. This suggests that the brain can recruit and reshape neuronal connections or unmask latent pathways to compensate for damage.
Applying Research Insights to Practice
The implications of these findings are profound for therapeutic practices. By understanding how the brain compensates for injury, practitioners can tailor their approaches to leverage neuroplasticity effectively. Here are some strategies:
- Encourage Active Rehabilitation: Early and active rehabilitation can stimulate neuroplastic changes, enhancing recovery after brain injuries such as strokes or surgeries.
- Utilize Non-Invasive Brain Stimulation: Techniques like transcranial magnetic stimulation (TMS) can promote plastic changes in the brain, aiding recovery in patients with motor or language impairments.
- Incorporate Multimodal Approaches: Combining imaging techniques such as fMRI with direct cortical stimulation can provide a comprehensive view of brain function and guide therapy decisions.
- Focus on Individualized Therapy: Understanding that each patient's brain adapts uniquely allows for personalized treatment plans that consider individual neuroplastic potential.
The Path Forward: Encouraging Further Research
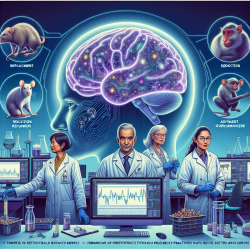
The study of neuroplasticity is still evolving, with many questions yet to be answered. Practitioners are encouraged to engage in further research to explore the full potential of neuroplasticity in therapeutic settings. Areas of interest include:
- The Role of Genetics and Environment: Investigating how genetic factors and environmental influences impact neuroplastic potential could lead to more targeted interventions.
- The Impact of Different Therapeutic Modalities: Comparing various rehabilitation strategies can help identify the most effective methods for promoting beneficial plastic changes.
- The Long-Term Effects of Neuroplastic Changes: Understanding how long-term changes in brain function impact overall health and quality of life is crucial for developing sustainable therapy models.
The potential applications of neuroplasticity research are vast, offering hope for improved outcomes across a range of neurological conditions. By staying informed and actively participating in ongoing research efforts, practitioners can continue to refine their skills and contribute to advancements in patient care.
If you're interested in exploring this topic further, I encourage you to read the original research paper: Neuroplasticity: Insights from Patients Harboring Gliomas.