Introduction
In a world where mental health is increasingly recognized as a crucial component of overall well-being, the challenges faced by low and middle-income countries (LMICs) like Nepal in providing adequate mental health services are stark. A recent study titled "Situational analysis to inform development of primary care and community-based mental health services for severe mental disorders in Nepal" sheds light on the barriers and potential solutions for improving mental health care in rural Nepal. This blog will explore how practitioners can leverage the findings of this study to enhance their skills and contribute to better mental health outcomes in their communities.
Understanding the Context
Nepal, like many LMICs, struggles with limited availability of mental health services, particularly in rural areas where the majority of the population resides. The study conducted focus group discussions and key-informant interviews in a rural district in western Nepal to explore resources, challenges, and barriers to developing evidence-based Comprehensive Community-based Mental Health Services (CCMHS).
Key Findings
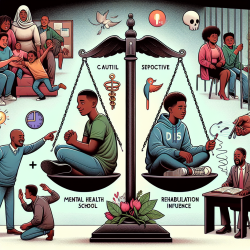
- Attribution of Mental Illness: Mental illness is often attributed to witchcraft, curses, or punishment for sinful acts. This cultural perception leads many to seek help from traditional healers rather than medical professionals.
- Lack of Services: Mental health services in medical settings are scarce, and primary care workers are often not equipped to handle mental health issues due to a lack of knowledge and inability to prescribe necessary medications.
- Support for Training: Health workers expressed a desire to upgrade their skills through resources like the mental health Gap Action Programme (mhGAP).
- Technological Barriers: While there is support for using mobile technology to deliver mental health services, there is a significant gap in familiarity with such technologies among health workers.
- Community Support: There is strong support for developing patient support groups and involving community resource persons in mental health service delivery.
Implications for Practitioners
For practitioners looking to improve their skills and contribute to better mental health outcomes, the study offers several actionable insights:
- Embrace Cultural Sensitivity: Understanding the cultural context of mental illness is crucial. Practitioners should work to bridge the gap between traditional beliefs and medical practices, potentially collaborating with traditional healers.
- Advocate for Training: Practitioners should advocate for and participate in training programs like mhGAP to enhance their ability to diagnose and treat mental health disorders effectively.
- Leverage Technology: While technological barriers exist, practitioners should explore ways to integrate mobile health solutions into their practice, potentially improving access to care.
- Foster Community Engagement: Building patient support groups and involving community resource persons can enhance the reach and effectiveness of mental health services.
Encouraging Further Research
While the study provides valuable insights, there is a need for further research to develop and implement a unified model for community-based mental health services in Nepal. Practitioners are encouraged to contribute to this research effort, helping to identify best practices and scalable solutions.
To read the original research paper, please follow this link: Situational analysis to inform development of primary care and community-based mental health services for severe mental disorders in Nepal.